having a child is not always as easy as it seems…
Many couples dream of starting a family, but when months -and sometimes years- go by without success, doubts, frustration and many questions begin to arise. One of the most frequent is: ‘Will we have a problem of infertility… or sterility?’ Although both words are used as synonyms in everyday conversations, in medicine they have different meanings. Understanding the difference not only helps to name the problem, but also points the way to a possible solution.
Infertility or sterility? It’s not the same thing, even if it looks like it
Sterility refers to the impossibility of achieving pregnancy. That is, fertilisation of the egg by the sperm does not occur. Infertility, on the other hand, implies that fertilisation does occur, and implantation may even occur, but the pregnancy does not succeed or ends in gestational loss (Practice Committee of the ASRM, 2021). Both situations can be primary (when a pregnancy was never achieved) or secondary (when there were previous pregnancies, but another pregnancy is not achieved). Knowing which one it is is key, because the causes, the emotions involved and the solutions may be different.
The causes: why does it happen?
In women
When it comes to female infertility, the most common causes are ovulatory problems (such as polycystic ovary syndrome), blocked tubes, uterine disorders or endometriosis (Malhotra et al., 2021). In the case of female infertility, the situation is usually more related to egg quality, more subtle hormonal problems, embryo implantation failure or repeated miscarriages, especially in women of older reproductive age (De Cherney et al., 2022).
In men
In men, sterility is often related to low sperm production, alterations in sperm shape or motility, and even azoospermia (total absence of sperm), which can have genetic or hormonal causes (Krausz & Riera-Escamilla, 2018). Male infertility, on the other hand, may be related to sperm that are present, but have DNA damage, functional alterations or difficulties in properly fertilising the egg (Agarwal et al., 2020).
Much more than a medical diagnosis: the emotional impact
Behind every diagnosis there is a story, a partner, an illusion. Infertility and sterility do not only affect the body, they also have a strong emotional impact. Anxiety, grief, guilt and even silence can become part of everyday life. According to Greil et al. (2011), the psychological impact is comparable to that of chronic diseases. Emotional support must therefore go hand in hand with the medical diagnosis.
What options do we have today?
The good news is that reproductive medicine has come a long way. Today we have multiple tools that allow us to treat both infertility and sterility successfully.
Some of the most common solutions are:
- Ovulation induction using hormonal drugs.
- Gynaecological surgery (e.g. to treat fibroids or endometriosis).
- Assisted reproductive techniques, such as:
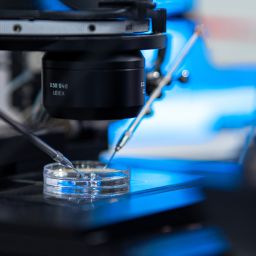
- Intrauterine insemination (IUI).
- In vitro fertilisation (IVF).
- Sperm microinjection (ICSI).
- Egg or sperm donation, in case of severe failures.
- Preimplantation genetic diagnosis (when there is a history of hereditary diseases or recurrent miscarriages).
Final message
If you are going through such a process, we want you to know something: you are not alone, you are not alone. Whether it’s infertility or sterility, the important thing is to seek answers, get the necessary tests and have a team that listens to you and accompanies you. Today there are solutions. But it is also important to take care of the process, to talk about what hurts and to ask for help if you need it. Fertility is not just a medical issue; it is also a deeply human story.
References
– Agarwal, A., et al. (2020). A unique view on male infertility around the globe. Reproductive Biology and Endocrinology, 18(1), 37.
– De Cherney, A. H., et al. (2022). Current Diagnosis & Treatment: Obstetrics & Gynecology (12th ed.). McGraw-Hill Education.
– Greil, A. L., et al. (2011). The experience of infertility: A review of recent literature. Sociology of Health & Illness, 33(1), 1–18.
– Krausz, C., & Riera-Escamilla, A. (2018). Genetics of male infertility. Nature Reviews Urology, 15(6), 369–384.
– Malhotra, N., et al. (2021). Role of endometriosis in infertility. Journal of Human Reproductive Sciences, 14(1), 7–16.
– Practice Committee of the American Society for Reproductive Medicine. (2021). Definitions of infertility and recurrent pregnancy loss. Fertility and Sterility, 116(6), 1360–1361.