Human papillomavirus (HPV) is one of a group of more than 200 related viruses. Some of these infections originate from anal, vaginal or oral sex, i.e. sexually transmitted diseases (STDs). HPV infection is estimated to have an overall prevalence of 10% in the female population of reproductive age (1).
This specific virus is differentiated into two types, low-risk and high-risk.
The low-risk type of HPV usually causes warts on different parts of the body, from the genitals and anus to the throat or larynx, causing respiratory problems. However, as specified by the US National Cancer Institute, they ‘rarely cause cancer’ (2).
More dangerous conditions are caused by high-risk HPV. They can cause several types of cancer, and there are about 12 types. Two of them, HPV 16 and HPV 18, cause most HPV-related cancers (3). These include anal cancer, cervical cancer, oropharyngeal cancer, penile cancer, vaginal cancer and vulvar cancer.
This is one of the most prevalent and recurrent infections in humans. Most people who have had sexual intercourse have been infected with the virus at some time. It is common for the immune system itself to control these infections and be able to clear them within a year or two (2).
In addition, vaccination campaigns against human papillomavirus (HPV) are common in developed countries. These vaccines prevent HPV infections and, consequently, prevent different types of HPV-associated cancers.
HPV symptoms in men: How do you know if you have it?
One of the major complications of HPV is the associated symptoms. It is known as the silent virus, as it is difficult to find an obvious ailment. In fact, the Center for Disease Control and Prevention notes that most people ‘have no symptoms or health problems’ (4). Only 10% of the time that this virus manifests itself can be seen as ailments.
It is through small genital warts, skin or mucosal changes that often go unnoticed. This is more accentuated when HPV is high risk.
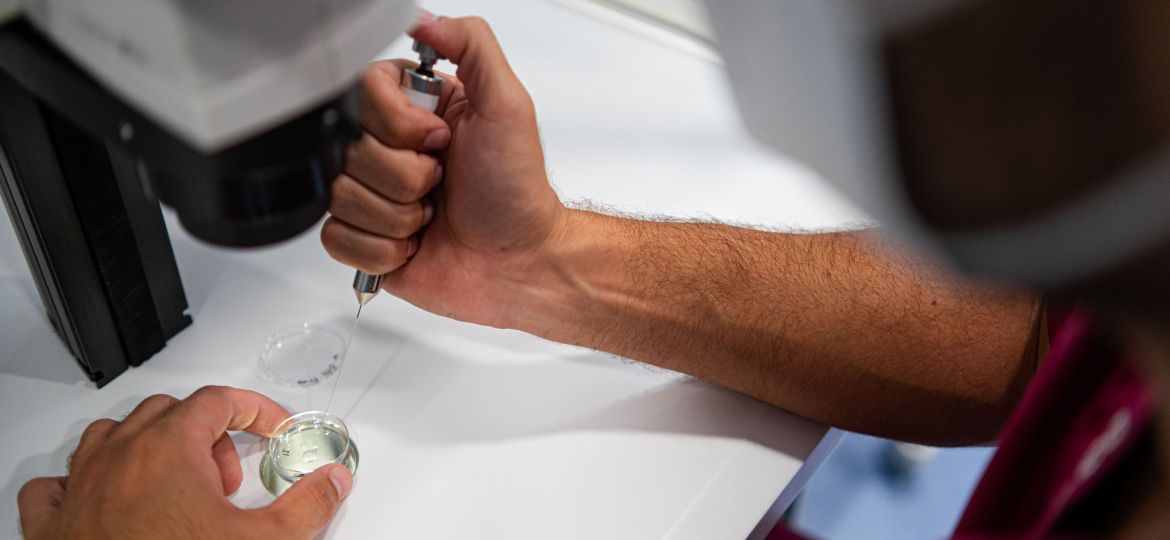
It is therefore recommended to see a specialist regularly. Although there is no existing test to detect this infection, there are visual examinations to detect warts or lesions, swab tests in specific cases, biopsy of suspicious lesions if there are signs of abnormal cells, and DNA testing to detect high-risk strains.
Impact of human papillomavirus on fertility
Sexually transmitted infections have a direct impact on human fertility. Although commonly linked to female reproductive health, they also affect male fertility, as they can induce an increase in sperm DNA fragmentation.
However, several observational studies among HPV-infected and uninfected infertile men have not found a direct relationship between infected patients and altered seminal parameters, such as decreased progressive motility or altered seminal pH. Semen parameters obtained after sperm selection procedures were similar to those generally observed in non-infected infertile patients (5).
Several studies have shown that the virus is transmitted vertically, as it can infect the birth canal, the placenta and the different fluids that come into contact with the foetus. Some studies have found that men without symptoms of infectious diseases or genital warts had part of the virus genome in their semen, and specifically fragments of viral DNA dispersed in different regions of the sperm morphology (head region and mid-region). According to this, the possibility that these viruses can be transmitted not only to the partner but also to the offspring, unnoticed, increases, as they can become asymptomatic carriers (7).
Other research concludes that the available evidence is still insufficient to draw definitive conclusions about the impact of HPV infection in women (6). However, when infection is present in the male partner, there appears to be a negative effect on the live birth/ ongoing pregnancy rate and an increased rate of miscarriage. This finding should be interpreted with caution, due to the very low quality of the supporting evidence (6).
Findings on human papillomavirus and fertility
This panorama allows us to draw some conclusions to be studied:
1) More studies need to be designed to provide solidity to those previously presented.
2) A field is opening up for research into the mechanisms of action of HPV in male semen, mainly, and how the product of fertilisation may be compromised.
3) A significant percentage of reported cases of loss of fertility, labelled to date as of unknown origin, could be solved by new semen washing techniques (8) (modified swim-up with the addition of heparinase-III) or by prophylactic male vaccination.
Bibliography
(1) FertilityandSterility Vol.95,No.5,April2011 1845 doi:10.1016/j.fertnstert.2010.11.047 Copyrightª2011AmericanSocietyforReproductiveMedicine,PublishedbyElsevierInc.
(2) National Cancer Institute (n.d.). Human papillomavirus (HPV) and cancer. National Cancer Institute. Retrieved February 27, 2025, from https://www.cancer.gov/espanol/cancer/causas-prevencion/riesgo/germenes-infecciosos/vph-y-cancer.
(3) American Cancer Society (n.d.). HPV and cancer. American Cancer Society. Retrieved February 27, 2025, from https://www.cancer.org/es/cancer/prevencion-del-riesgo/vph/vph-y-cancer.html
(4) Centers for Disease Control and Prevention. (n.d.). About genital HPV infections. Centres for Disease Control and Prevention. Retrieved February 27, 2025, from https://www.cdc.gov/sti/es/about/acerca-de-las-infecciones-genitales-por-el-vph.html.
(5) Foresta, C., Pizzol, D., Bertoldo, A., Menegazzo, M., Barzon, L., & Garolla, A. (2011). Semen washing procedures do not eliminate human papilloma virus sperm infection in infertile patients. Fertility and Sterility, 96(5), 1077-1082. https://doi.org/10.1016/j.fertnstert.2011.04.009
(6) Assisted Reproduction Unit, 3rd Department of Obstetrics and Gynecology, ‘Attikon Hospital’, Medical School, National and Kapodistrian University of Athens, Athens, Greece; 2SEMEAR Fertilidade, Reproductive Medicine, Ribeir˜ ao Preto, Brazil. 10.1002/uog.17550
(7) Zea-Mazo,J., Negrette-Mejıia, YA., & Cardona-Maya, W. (2010). Sexually transmitted viruses: semen and virus relationship. Actas Urologicas Españolas, Volume 34(10), 845-853. https://doi.org/10.1016/j.acuro.2010.07.002
(8) Silva Garretón, A., Mayer, M., Layus,O., Rey Valzacchi, G., & Gueglio,G. (2016). Male genital human papillomavirus infection. Rev. Hosp. Ital. B.Aires; 36(4): 143-149.






